Male circumcision reduces the risk of HIV acquisition by heterosexual men by up to 66%.

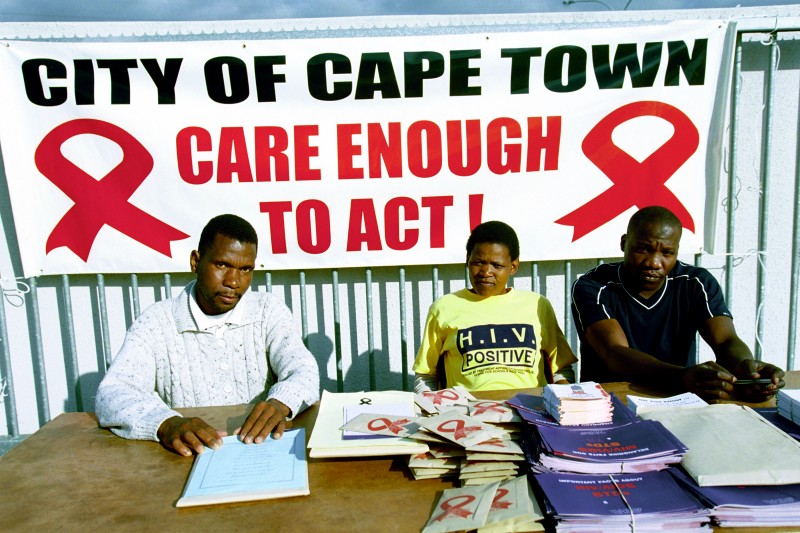
Photo Credits: Ray Witlin (L), Trevor Sampson (R)
Why is male circumcision important?
Male circumcision is the surgical removal of all or part of the foreskin of the penis. It can be done as a religious or traditional ritual, or as a medical procedure to prevent and treat infections, injury, or abnormalities. Observational studies since the 1980s have suggested that circumcision provides a protective effect from HIV infection. More recently Randomizec Control Trials (RCTs) have reported similar results.
Does it work?
- Male circumcision among heterosexual men reduced HIV acquisition by up to 66% over 2 years. All three randomized controlled trials (RCTs) included in this review were stopped early because of the significant findings supporting the protective effects of male circumcision.
Equity: Does circumcision work in the disadvantaged?
- There is no evidence to suggest that circumcision would be less effective in disadvantaged populations.
Intervention Delivery
- All of the included studies performed medical circumcision under local anaesthesia by local general practitioners experienced in circumcision or the study clinician operating in the study clinic.
- Each study required at least 3 follow up visits, at 1, 3, 6, 12, and 21-24 months.
Population and Setting
- Three large RCTs were conducted in South Africa, Uganda and Kenya.
- All included trials were conducted in low- or middle-income African countries . One study was conducted in an urban setting, one semi-urban, and one rural.
- The South African study included 3274 participants, the Ugandan study had 4996 participants and Kenya had 2784 participants.
- Participants were sexually active men between the ages of 15 and 49 who were HIV uninfected at enrollment.
Summary of Findings [SOF] Tables: Circumcision for preventing heterosexual acquisition of HIV in men.
Patient or population: Sexually active heterosexual HIV uninfected men
Settings: Kenya, South Africa, and Uganda
Intervention: Circumcision
Comparison: No circumcision
Outcomes
| Anticipated absolute effects per year | Incidence Rate Ratio (95% CI)
| No of Participants (studies)
| Quality of the evidence (GRADE)
| |
Risk without circumcision (Control) | Risk difference with circumcision (95% CI) | ||||
HIV incidence (0-12 months) | 16 per 1000 | 8 fewer per 1000 (from 4 to 10 fewer) | IRR* 0.50 (0.34-0.72) | 10,908 (3 studies) | High |
HIV incidence (0-24 months) | 10 per 1000 | 5 fewer per 1000 (from 4 to 7 fewer) | IRR 0.46 (0.34-0.62) | 10,908 (3 studies) | High |
Adverse Events: The rate of adverse events for medical circumcision ranged from 1.72% to 7.65%. Reported adverse events included: pain, excessive bleeding, infection, damage to the penis, delayed wound healing, insufficient skin removed, problems with urinating, problems with appearance, and swelling. All three trials found that men in the circumcision group were more likely to practice risky sexual behaviors than controls. | |||||
About quality of evidence (GRADE) | |||||
* IRR = incidence risk ratio
| |||||
Relevance of the review for disadvantaged communities
Male circumcision reduces the risk of HIV acquisition by heterosexual men by up to 66%.
There is no evidence to suggest that circumcision would be less effective in disadvantaged populations.
Findings | Interpretation |
Equity - Which of the PROGRESS groups examined | |
Participants in the three RCTs were from South Africa, Uganda, and Kenya. All participants were sexually active men between the ages of 15 and 49. All the men were HIV uninfected at enrollment. | There is no evidence on the effectiveness of circumcision as a preventive procedure prior to the start of sexual activity but this is something that could be explored in future studies. The men most likely to benefit from a medical circumcision intervention should be selected. |
Equity Applicability | |
Circumcision in the included studies was performed using commonly used surgical techniques and local anaesthesia. In many countries, circumcision is performed by a traditional healer as part of the rites of initiation into manhood | The results of the study are specific to circumcision performed as a medical procedure and do not support traditional circumcisions which have higher rates of adverse effects. Policymakers who want to implement a circumcision intervention will need to find a way to incorporate the medical procedure of circumcision into these traditional customs. Patients undergoing medical circumcision need to receive information about wound care and identifying possible complications. |
All three trials were conducted in areas with high rates of HIV transmission. | The risk of HIV infection in the population should be considered before planning a medical circumcision intervention. There is no information yet to describe the effectiveness of male circumcision on female partners. |
Cost-equity | |
The review does not comment on the cost-effectiveness of medical male circumcision. | The cost-effectiveness of the intervention needs to be explored. Policy makers need to consider the costs included in the medical procedure, including local anaesthetic and follow up care when needed. The costs of HIV infection should be weighed against the cost of medical circumcision. This review reports that the number needed to treat is 62 to prevent 16 HIV infections assuming a control risk of 3% (30 per 1000) |
Monitoring & Evaluation for PROGRESS groups | |
Longer term evaluation of the effectiveness of medical circumcision is needed. Other studies should examine the feasibility of implementing this intervention in different contexts as well as the related social and cultural issues. | All three trials found that men in the circumcision group were more likely to practice risky sexual behaviours, such as unprotected sex, than controls. During the two year study follow up period circumcised men were protected but more follow up studies are needed to determine if circumcision benefits persist long term. |
Comments on this summary? Please contact Jennifer Petkovic.
